Straight answers to a straightforward question
Have you had a baby (or several?) Sex isn’t the same: loose, lax, less friction, opening sags and looks “..old.” Are you less able to orgasm with gusto? Thinking of a procedure to “…make things better?” Are you confused over the words “Vaginal Rejuvenation; “Vaginoplasty;” Vaginal Reconstruction;” Perineoplasty;” Laser tightening; Radiofrequency (RF) tightening; magnets and other toys to tighten..?!
Let’s honestly separate the wheat from the chaff… So-called “vaginal tightening procedures can be divided into the categories of surgical, vs. non-surgical. What is the difference?
Non-Surgical procedures are performed with what have been termed “Energy-Based Devices,” or EBDs. Of these there are 3 main types, laser, RF (radiofrequency), and magnet-based devices such as Emsella. All require 3 or more separate trips to the Clinic, cost ~ the same (~ $2,500-3,000), and the outcome of both are similar. You can bet that whichever device your local Plastic Surgeon or Gyn. or MedSpa has purchased will be described as the “best one on the market,” according to the facility. EBDs require very little training (“…just follow the instruction book…”) and may be performed by a clinician not trained in surgical tightening, and even by just a nurse or technician. While these techniques have proven to be of decent help with mild to modest urinary incontinence, and can be used in post-menopausal women to enable the vaginal skin to stretch better and become more resilient, they in no way narrow the vaginal caliber, tighten the fascia, re-connect the muscles, remove scar tissue, rebuild and strengthen the vaginal opening, vulvar vestibule and perineum, or change the appearance of the vaginal opening or perineum. BUT, laser and RF devices do “rejuvenate” by increasing the amount of elastin and collagen fibers in the skin. If “…beauty was skin deep” (or if vaginal tightening could be accomplished by only making the vaginal skin a bit more stretchy,) they would be fine for tightening. But, unfortunately, they are not, and usually are used for vaginal tightening only by those providers who have not yet learned the skill of surgically tightening the vaginal barrel. They are however legitimately used in conjunction with surgical tightening to aid in urinary incontinence problems.
Surgical procedures that result in vaginal tightening are best performed usually by either a Gynecologist or Urogynecologist who has additionally been trained specifically in vaginal tightening (“vaginal reconstruction” or “vaginoplasty”) in either a specialized training program, or has trained themselves by performing dozens and dozens of these surgeries. This is an art that includes a mindful aesthetic repair of the opening, and is far different from the standard “Posterior Repair” or “A&P Repair” performed by general Gynecologists or Urogynecologists. Certainly, additional work with a Pelvic Floor Physical Therapist will add both strength and duration to the specialized surgical work.
How does one find such a specialized surgeon? While a very occasional P.S. (Plastic Surgeon) has been trained to work deep within the vagina, this type of surgery is the purview of Gynecologic or Urogynecologic surgeons. However, only a small group of these surgeons have either spent years and years perfecting their technique, or have been specifically trained by one of the acknowledged trainers for these [tightening] techniques worldwide. Both myself and Drs. Davis Matlock, Marco Pelosi II and III, and Red Alinsod have been training for >10 years. Dr. Alex Bader in the U.K. and Europe has been training surgeons for ~ 5 years, and Dr. Troy Hailparn in San Antonio TX has been training for ~ 2 years. Both myself and Drs. John Miklos and Rob Moore in Atlanta, GA have had occasional Fellows that we have trained. So… the consumer must carefully do her “due diligence,” looking carefully at websites of surgeons to ascertain his or her experience, training, and specific interest in the specialty of vaginal tightening.
Another valid question nowadays is the best kind of anesthetic technique for a vaginoplasty/vaginal reconstruction/vaginal tightening procedure. While traditionally performed under “general” (asleep) anesthesia in a hospital or surgical center, beginning ~ 10 years ago, Dr. Red Alinsod in Laguna Beach, CA, followed a year later by Dr. Michael Goodman to the north in Davis, CA, began performing these procedures in their office surgical suites under “local” (awake) anesthesia, and until recently were the only surgeons in the U.S., and perhaps the world, performing true, complete vaginal tightening on an awake patient. Presently, a small number of both Dr. Goodman’s and Dr. Alinsod’s trainees are beginning to work “…under Local…” In my personal opinion, local anesthesia is superior to general/asleep for several reasons. While the exposure and ability to adequately perform the work is now present whatever the anesthesia because of new instrumentation, local anesthesia is certainly easier on the body, and the recovery far simpler. Additionally, performing surgery under “local” gets rid of the large additional expenses of hospital or surgical center, and a separate anesthesiologist’s fee. The most important benefit for “local” for me personally, is that I can do a better job of reconnecting the muscles and tightening the vaginal barrel under local. This is because of one of the risks of vaginoplasty (which is really a “levatorplasty,” wherein the levator-aka “Kegel’s- muscles are re-approximated in the midline in the vaginal floor to both support, buttress, and narrow the mid-vagina. A risk of this specific procedure when performed on an asleep patient is the trapping of one of the nerves in these muscle bundles producing what is termed as “levator spasm,” producing ongoing pain in the vaginal floor. For this reason, “traditional” Gyn or Urogyn surgeons operating in the hospital on an asleep patient will not perform a true, aggressive vaginal tightening operation consisting of levator muscle re-approximation. However, if performed under “local” on an awake patient, the surgeon can be more aggressive in the tightening. In this situation, if a nerve is temporarily trapped, the patient will immediately feel it, have pain, and let the surgeon know so that (s)he can immediately remove and replace the suture, resulting in a better performed, tighter, and more complete reconstruction.
Hopefully you are now well educated, and can make an informed decision regarding the type of procedure best for you personally to result in more vaginal friction, and a more enjoyable sex life!
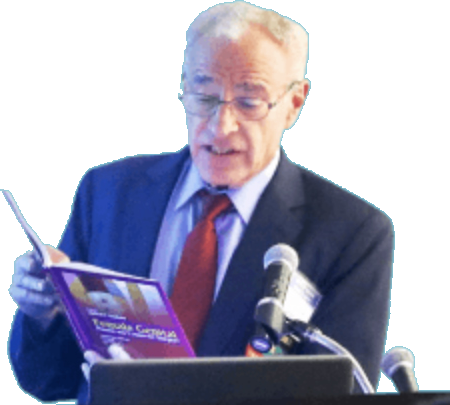
–Michael P Goodman, MD, FACOG, IF, AAACS
Davis, Northern CA, USA