Hysterectomy (“hyst.”) is one of the most common operations undergone by women. Uterine Artery Embolization (“UAE”) is finding increasing popularity as an alternative to hysterectomy for therapy of benign tumors of the uterus and abnormal uterine bleeding in women who, for a variety of reasons, wish to retain their uterus.
2. “Why do you feel I need a hyst (or UAE); what will it accomplish? [Is this what you wish to accomplish?]
3. “What are other avenues–surgical, radiological, nonsurgical, hormonal, etc., for accomplishing what I wish? What are the pros and cons of each?” [Do any of these alternatives seem to warrant further exploration?]
4. How long will I be in the hospital or outpatient facility? What about pain? When can I return to general activities? Sex? Work? What are the risks?” [Is this acceptable to you?]
5. “With this procedure, will I require hormonal therapy afterward? If yes: What do you have in mind?” [Make sure that you fully understand this before the procedure. If ovaries are to be removed, make sure, in addition to estrogen, that testosterone is provided].
6. “In what ways might this procedure effect me sexually?”
7. “If you are having a UAE, be sure to make your radiologist aware that you expect him to be careful and selective, occluding the uterine arteries distal to (“after”) the blood vessels that supply other parts of the pelvis exit from the uterine artery.
What To Expect And How To Deal With It With either UAE or hyst (whichever the approach: abdominal, vaginal, laparoscopic or supracervical) you are having a surgical procedure involving a very vulnerable area. Be prepared for this. Discuss it with yourself, your partner, your physician and your therapist if applicable. How do you feel about it? What about your ovaries? Will it be best to leave them in and let them function (of dysfunction) as the case may be? Or to remove them, substituting estrogen and testosterone and possibly progesterone–which could either be a hassle or immensely beneficial, depending on how those ovaries are presently functioning (more about this later).
1. Loss of your uterus (hysterectomy): Be prepared to experience this as a loss. A part of you–the organ where your children grew (or perhaps where you wanted them to grow if you are involuntarily childless) is being removed. On the other hand, if there is bleeding, pain, etc.–this may be a huge relief.
2. Loss of ovaries: Same as above. If your ovaries are synonymous with your femininity–think it over seriously and discuss with a therapist or your gynecologist if the issue is unresolved. A good rule of thumb: If you are psychologically attached to your ovaries and they help define your femininity, leave them in! If, at any age, there are serious disturbances stemming from hormonal dysfunction (e.g. severe PMS, menstrual migraine, etc.) consider taking them out and going on HT. On average, your ovaries run out of eggs and hormones +/- age 45-55, so if you are over 45, you may consider removal and estrogen/testosterone which will usually guarantee a smooth transition and eliminate peri-menopausal/menopausal symptoms entirely (you won’t go through menopausal changes, as you are already “transitioned” to hormone therapy). Later, after you are stabilized, you can work on a slow hormonal taper-down if you wish.
3. UAE: Why does a heart attack hurt? Because muscle is being deprived of blood and oxygen and is dying. The same with the uterine muscle in UAE. It can hurt like H for several days. Be prepared with pain meds and NSAIDs. Additionally, understand if the embolization is not as “selective” as hoped, you may have significantly diminished sensation in vaginal, vulvar and clitoral areas.
4. Sexual functioning: Not infrequently, for factors related to the reason you are having your procedure in the first place, you and your partner may have grown sexually distant. Then, for a period of time (4-6 weeks; significantly less with UAE and supracervical lap hyst), you won’t be able to enjoy intercourse. Initially you will be fatigued; you will be hurting–both hyst and UAE are a little like getting run over by a truck. Discuss this with your partner. Openly acknowledge the situation if you have grown sexually distant. Do you and he wish to be closer? Discuss this. It is not at all unusual for midlife women and women with uterine maladies to have a significant diminution in desire for a variety of reasons (hormonal changes, poor sleep quality and fatigue, pain, bleeding, etc.). Get your hormones balanced with estrogen and testosterone replacement if your ovaries have been removed, and possibly the same (perhaps even adding progesterone) if you still have ovaries but are perimenopausal. This and the resolution of the medical problem will help, but don’t necessarily expect the desire to come all back. It frequently doesn’t. You can still work your way back to enjoyable and fulfilling sexual relations.
Some ideas:
a) Even though you may not be able to have intercourse, you and your partner can still engage in single or mutual self-pleasuring, fantasy, oral sex, touching, kissing, etc.
b) SCHEDULE “DATES”! This really takes the pressure off both of you. Schedule “intimate time” at least once (hopefully twice a week) in bed, at a time when you can be private and when both of you are fresh. This is a time for intimacy, for sharing, for reestablishment. A time for communication, for new directions, for erotica and fantasy and perhaps arousal. And, who knows “desire” may follow…
Remember: What determines post-procedure sexual functioning is pre-procedure functioning and preparation.
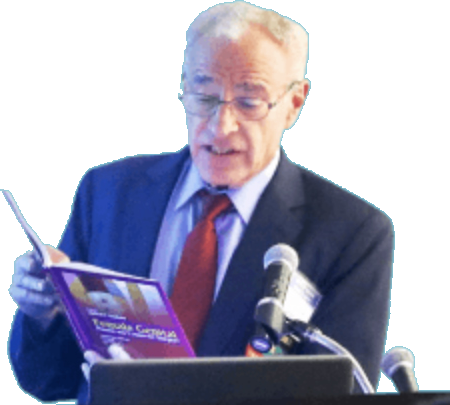
The more prepared you are, the more you have thought about it and discussed it with your family, doctor and counselor, the better you will do afterward. An excellent reference for women about to undergo UAE or hysterectomy is “A Gynecologist’s Second Opinion” by William H. Parker, M.D. (Plume Books, 2003 edition).